Updated October 19, 2022 at 10:33 AM ET
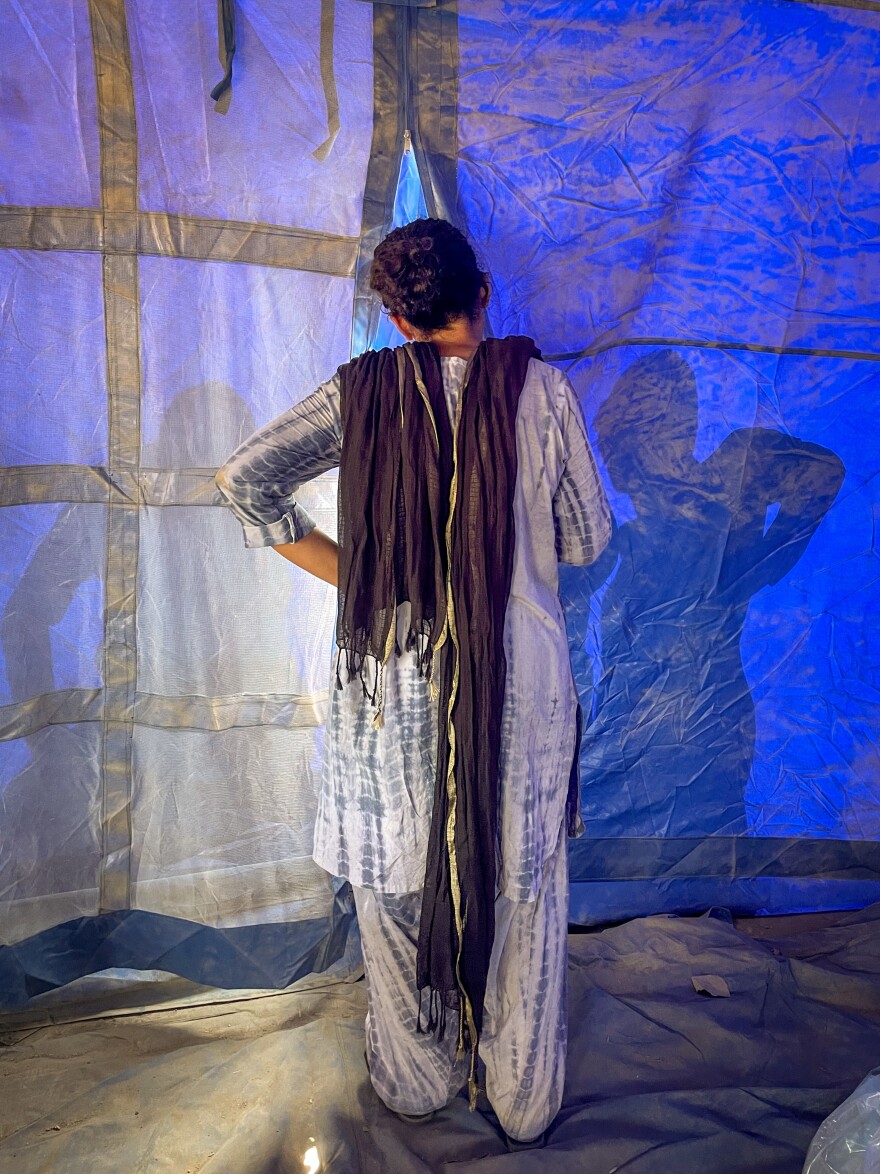
Neha Mankani peeks into tarpaulin tents pitched in rows between cotton fields near the southern Pakistani village of Sheikh Daro. They flap in a hot wind that whips up dust that grits the eyes and coats the tattered clothes of the men, women and children who've been living here since they were made homeless by Pakistan's devastating floods this summer.
"I'm looking for pregnant women, and I'm trying to mobilize them so they can come to my makeshift clinic," says Mankani, a midwife who leads the Karachi-based Mama Baby Fund. The small charity has been running pop-up clinics for pregnant women in flood-affected areas, like this encampment established by a Canadian aid group,the Al-Qaim Charity Foundation.
The needs are unimaginably vast in areas where Pakistan was pummeled by torrential monsoon rains for weeks. Officials estimate more than 7 million people were made homeless. Several hundred thousand of them, at least, are living in encampments and by roadsides across southern Pakistan. Among those affected, says the U.N.'s Population Fund, are nearly 130,000 pregnant women in need of urgent health services.
Those women are particularly vulnerable. Even before the floods, Pakistan had one of Asia's highest maternal mortality rates. In the southern province of Sindh, one of the worst affected by the floods, the U.N. estimated that more than a fifth of all people in the province were facing high levels of acute food insecurity and were in need of urgent action to shore up their food consumption.
"The most urgent problem we have is malnutrition," says Farhana Menon, a senior official in Sindh's provincial health ministry, where she oversees the needs of pregnant women in particular. Menon says the ministry has dispatched ambulances to encampments, so they can ferry out women who need to give birth, but the need is enormous.
"Some people have given birth in schools. They've given birth in boats. They've given birth in tents," says Mankani, referring to displaced women who are sheltering in public schools and others who rely on boats for transport because their villages are surrounded by floodwater.
One of Mankani's challenges is convincing women in conservative areas that she can be trusted to see and touch their swollen bellies. So she's bought along a lure: She tells women crammed in a line for drinking water that pregnant women can have an ultrasound if they visit her clinic. It's a special treat in rural areas where even in ordinary times, health care is ramshackle. "It's going to be a pull to get people to come to my clinic," she explains.
Mankani need not have bothered.
A few minutes after she speaks to the women, she returns to her makeshift clinic, which her team has set up in an empty blue tent at the encampment's entrance. There's already a crowd of women and children waiting outside. "Oh! I didn't expect so many people!" she exclaims and rushes in. In one corner, volunteers have placed a charpoy, a daybed made from wood and rope, to examine patients.
Mankani beckons the women in. "One at a time!" she calls.

A pregnant woman walks in, holding a wailing toddler. Mankani asks her to lie down, raises her colorful, thin cotton shirt. She presses her Doppler – a fetal heart monitor – against the woman's swollen belly. A steady thump emerges. The baby's fine, but the woman needs support. She's dizzy, and Mankani rummages through her boxes to give her oral rehydration salts and iron pills.
Mankani turns her attention to the crying toddler. The boy's mother explains he's not getting enough food. He's got diarrhea, too. There's an added complication: He's got cerebral palsy and has been having seizures.
The boy needs a doctor, not a midwife, but Mankani's all they've got. She gives the boy nutritional supplements that she pulls out of a stack of boxes heaped in a corner.
A rhythm emerges. A volunteer calls in one woman at a time from the noisy crowd outside. Through social worker Moomal Mallah, who translates from Sindhi, the local language, Mankani chats with her new clients while checking for fetal heartbeats. Maine-trained midwife Jahan Zuberi, who works alongside Mankani, does the same.
Mothers and babies need help as well. The midwives dole out vitamins, iron supplements, food supplements. Infant formula.
The mobile ultrasound — which was meant to lure women in — keeps breaking down in the heat.
Thirty-year-old Shehzadi walks in. She's only got one name, like many people in Pakistan. She's thin, with a small belly – five months along. And she's worried about where she'll give birth.
"She hopes she'll be back in her village before this one is born so she can give birth at a facility," Mankani explains. "If not, she says she'll have to give birth in the camp."

But Shehzadi is probably going to be in this encampment for months. The water still hasn't receded in some parts and rebuilding will be expensive. So Mankani gives Shehzadi a life-saving package: a delivery kit, with a sterile plastic sheet to give birth on. A razor to cut the umbilical cord. There's nappies for the baby. There's medicine for Shehzadi to prevent hemorrhage.
Then, a man calls out from outside the tent: Mankani's team has to move. The encampment's religious leader wants to pray in this specific tent, and he won't consider using another. "We're going to have to move! How will we move all our stuff?" Mankani asks fellow midwife Zuberi.
But they do. They shift their things to a nearby empty blue plastic tent – it's an informal school for displaced children, but the day's classes have ended, leaving a blackboard scrawled with the Urdu alphabet in one corner.
The crowd of waiting women follow them. They've been waiting hours and it's hot — around 110 degrees.
Many of the women are waiting for nutritional supplements for their little ones, Safoora, a woman who guesses she's 30 years old, has come with her seventh child. Her baby, Samira, wears grubby clothes concealing a thin, light body. Safoora says Samira has become feverish and sick and keeps throwing up the little food she can give her. Safoora tries to breastfeed, but she doesn't have much milk. She begins crying. "We need help," she says. "I want to save my baby."
One woman impatiently holds a crying, writhing baby to the new tent's fly-screen window to get the midwives' attention. She says the baby, Aziza, needs formula. Mankani, feeling the belly of another pregnant woman, calls out from inside the tent, "You should breastfeed her!"
The woman shakes her head and calls back to Mankani, "The mother is dead!"
Mankani walks to the tent window and the woman explains she is Aziza's aunt. The baby is too young for food. Mankani packs a plastic bag full of formula and hands it to the woman.
Through another tent flap, a little blonde girl gestures and waves at the midwives. "That's not a pregnant woman," says Mankani, shaking her head.
The girl holds a baby to the flap for the midwives to see. He's so small, he looks like a doll. Mankani quickly lets the girl in. Her name is Ruksana; her brother is Zaman. Ruksana, like most women and girls here, is illiterate, and she doesn't know her age or the age of her brother. He was born last winter, she says.
Mankani opens his mouth to check for teeth. "He's one-and-a-half, at least," she says, but it's hard to believe, because Zaman looks so small, so fragile.
Mankani gives the girl a bag full of vitamins and a powdered food supplement for them both. Ruksana touches Mankani's feet to show gratitude. With her brother on her hip, she weaves back out of the tent.

It's time for a break.
Mankani sits down on a daybed near a solar-powered fan.
For seven years, Mankani has run midwife clinics for underserved women in Pakistan. But this – "this is terrible," Mankani says. "It's the worst I've seen."
It's the blazing heat in the open tents. The desperate need of mothers who've long been poor and malnourished, whose children are vulnerable to starvation and sickness – particularly from stagnating water that brings with it diarrhea as well as mosquitoes bearing dengue and malaria. Witnessing people struggle after losing everything to floods that were exacerbated by climate change that they've done nearly nothing to contribute to.
And Mankani knows she's only treating a fraction of the women and children who need her care.
She makes peace knowing she's doing all she can. "I just have this philosophy that all the women I see myself – I know are getting respectful care," she says. That's part of why she does this, she says. She gives a tired laugh. "And I'm just a little crazy."
Later the evening, Mankani messages from the fleabag hotel where she's staying in the nearby hub of Dado. She tells me her team saw 80 women in the camp in one day. She says the next day, she'll do it again.
Copyright 2024 NPR. To see more, visit https://www.npr.org.




