(This story was originally published in the Idaho Capital Sun.)
Patients treated in emergency rooms. Small community hospitals calling around for a place to send their critically ill patients. Nurses so burned out that hospitals offer them cash to take extra shifts. And a delta-fueled COVID-19 fire raging out of control from coast to coast.
Idaho has entered a fourth surge in the coronavirus pandemic. But this one is different from the third surge that pushed Idaho hospitals to the brink of “crisis standards of care,” when hospitals are forced to choose which patients get life-saving medical care.
“The overall trend is bad. It’s looking worse than the December, January surge. We’ve had a sixfold increase (in these) COVID numbers over the past six weeks, and a doubling from two weeks ago,” Dr. Jim Souza, chief physician executive for St. Luke’s Health System said Thursday.

He and other Idaho health care leaders are pleading with the public — at every news briefing and every public engagement — to get vaccinated.
Idaho’s uptake of the COVID-19 vaccine has increased in the past six weeks. But it remains too low for Idaho to have widespread protection. Many Idahoans were infected last year and recovered; but the virus now circulating in Idaho is different.
Data obtained and analyzed by the Idaho Capital Sun show that severe illness is on a steep rise. It is filling hospital beds faster than at any time during the pandemic.
Delta is adding to ERs, filling Idaho ICU beds
It’s unclear whether the delta variant just spreads more quickly, or if it also makes people sicker.
But the variant overtook all other types of COVID-19 virus in Idaho in a matter of weeks, based on Idaho Bureau of Laboratories genetic sequencing of virus samples.
That spread coincides with a steep uptick of people going to emergency rooms with COVID-19 symptoms, and an even steeper increase in hospitalizations for COVID-19.

Idaho’s intensive care units are now as full as they were in December, based on federal data reported by the hospitals. And the share of ICU beds taken by patients with COVID-19 — 36% — is nearing its December peak.
The trajectory, though, is much steeper than it was in the fall surge.
The hospitals are contending with other pressures, too: heart attacks, strokes, traumatic injuries, infections and now, the out-of-season arrival of RSV, the respiratory syncytial virus that is responsible for more child hospitalizations than any other cause.
Some of Idaho’s largest hospitals are once again pausing non-emergency procedures, to keep from buckling under the added strain of more sick COVID-19 patients.
Kootenai Health in Coeur d’Alene said last week that it had to postpone those procedures for six or eight weeks.
“With the trending cases climbing, we are rapidly exhausting our staffing resources,” Kootenai Health CEO Jon Ness said in the hospital’s news release announcing the pause. “The COVID-19 hospital census is rising at a faster rate than it did last winter. If this trend continues, in just five days we will surpass our previous COVID-19 high census from December 2020.”
The hospital said that, since the start of this latest surge, 97% of all hospitalized COVID-19 patients were unvaccinated.
St. Luke’s Health System also announced the cancellation of certain non-emergency procedures for several days this month at its largest hospitals — in Boise, Meridian, Nampa and Twin Falls. The system has seen a large increase in COVID-19 patients, who now make up 22% of its hospitalizations systemwide.
Nearly one-third of the patients at St. Luke’s in Meridian have COVID-19, the health system’s public data show.
Mark Snider, spokesperson for Boise-based Saint Alphonsus Health System, told the Sun last week that the system is “monitoring inpatient bed capacity and evaluating each appointment on a case-by-case basis.” Saint Al’s was not doing a “blanket pause” as of Wednesday, he said, “but may need to implement strategies to address capacity concerns in the future.”
Running low on nurses in Idaho hospitals
Souza and other health care leaders have said that these “elective” procedures are medically necessary. They should be done as soon as possible, to keep a tumor from growing or help someone who is in immense pain. But the hospitals have to make sure they can take care of people who arrive near death with COVID-19.
Kootenai Health’s incident commander said in its announcement last week that it is struggling to find enough nurses to care for the sickest patients.
The hospital had pulled employees off their other duties in clinics and outpatient areas to help with the hospital surge, it said.
“Kootenai Health leadership reached out to resources at the state level to request help” on Aug. 9, the news release said.
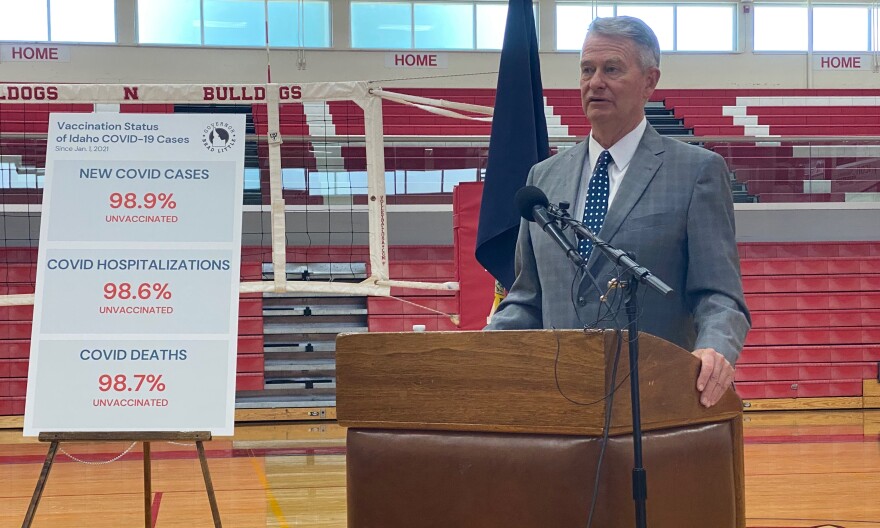
Gov. Brad Little said at a press conference Thursday, Aug. 12, that more Idahoans need to get the COVID-19 vaccine. That will help prevent interruptions in the coming school year, he said. He also pointed to hospitalizations as a reason to get vaccinated; they are almost all patients who aren’t fully vaccinated. (Kelcie Moseley-Morris, Idaho Capital Sun)
Idaho Gov. Brad Little said Thursday that he talked with National Guard leadership in recent days, about if and when he should re-deploy guardsmen to help with COVID-19 response. A reporter asked whether he expects to deploy the Guard in the near future. “Don’t be surprised,” Little said.
“The more work you have to do, the more people you need to care for, the more challenging it is,” Souza said. “Our ICU census is bursting at the seams. That means each individual intensive care doctor has to take care of a larger allotment of patients. … I just want to remind people that when you take a tired crew, and you say, ‘You know what? Just put 20 more pounds in your pack, and keep on walking,’ that takes some magical thinking to think you’re going to get the same output.”
He hopes it won’t lead to mistakes, or infections, or simply lead to St. Luke’s having to send patients elsewhere.
“I hope that’s where it stops — that you don’t get your call light answered as quickly, you don’t get that glass of juice that you want,” he said. “But I’m concerned it could go beyond that.”
Frontline worker in crisis? There is helpIdaho launched a dedicated, free hotline last year for frontline workers. It offers 24/7 crisis counseling and helps callers access short-term and longer term mental health care. Call 866-536-0239.
St. Luke’s Health System in early August offered certain employees bonus pay if they took on extra shifts.
Registered nurses, respiratory therapists and other health care workers would receive up to $2,500 if they signed up for, then worked, six additional 12-hour shifts between Aug. 1 and Oct. 2. Health care support services workers got the same offer, with a bonus of up to $1,500.
“To better meet scheduling targets while we close staffing gaps, an extra shift bonus program is in place for specific positions at St. Luke’s,” said Michelle Bartlome, St. Luke’s Magic Valley and Jerome public relations manager, in an email Friday. “At this time, the approved bonus program will run through Oct. 2, 2021 and is available for team members throughout St. Luke’s Health System.”
Former ICU nurse: ‘This … I won’t do this’
The vast majority of health care workers in local hospitals have been vaccinated against COVID-19. They are unlikely now to become sick enough to be hospitalized or die. But the past 18 months have taken a toll on them — and on the entire health care system.
More than 9,000 Idahoans have been admitted to a hospital with COVID-19. One in six was so critically ill, they were admitted to the ICU.
But there is no cure for the disease. Specially trained nurses, doctors and therapists can use machines and medications to keep a person in limbo between alive and dead. Sometimes they can sustain that limbo until the body starts to heal itself. Sometimes they can’t.
More than 900 people have died in Idaho hospitals from COVID-19 since last August, according to federal data. Health care leaders worry about their staff’s mental health. At work, they witness death and grief-stricken families; outside the hospital walls, they meet people who deny that reality.
The Idaho Capital Sun watched recently as hospital employees crossed paths with anti-vaccine protesters outside the St. Luke’s hospital in downtown Boise.The protest, on a sidewalk outside the hospital’s ER doors and ambulance bay, was one of several this summer at St. Luke’s and Saint Alphonsus health systems and Primary Health Medical Group. Those businesses will soon require staff to be vaccinated for COVID-19.
Some protesters held signs saying they were health care workers and didn’t want to be used to test “experimental” vaccines. All three vaccines currently authorized for COVID-19 by the Food and Drug Administration have undergone more than a year of testing in large-scale clinical trials. Half of the U.S. population has been vaccinated, with a miniscule number of serious adverse reactions.
A former ICU nurse told the Idaho Capital Sun she quit her job after the late 2020 surge.
She was working in a hospital in another state. It became a major COVID-19 hot spot, and the ICU ran out of beds, she said. Understaffing meant nurses were assigned too many patients, she said. She left the job soon after and returned to Idaho, her home state.
“I can’t deal with people (who deny the pandemic) and I refuse to take care of patients that, at this stage in the game, refuse to get vaccinated,” said the nurse, who did not want her name used. (The Sun confirmed her credentials.)
“I’d see their vaccination record in the chart,” she said. “I never used to care what the patient background was … drug user, incarcerated with a guard at the bedside, morbidly obese, (alcohol) abuser with dying liver … no problem. But this … I won’t do this.”
Meanwhile, hospitals around the U.S. are becoming overwhelmed.
Souza said two recent patients admitted at St. Luke’s were from coastal Oregon and from Oklahoma. The hospitals there couldn’t admit them, or find an open bed nearby, so the patients ended up hundreds of miles from home.
As the virus burns through pockets of unvaccinated people nationwide, the search for a staffed bed is getting more intense.
Just a few days before the Oklahoma patient was transported to St. Luke’s in Idaho, a hospital in Oklahoma City issued another plea to the public to get vaccinated. All its beds were full. And it wasn’t just that hospital, it said; it was the whole state.
Earlier in the week, the hospital said on Facebook that it had been forced to deny 121 requests to transfer patients into its care, because “we simply didn’t have space.”
Almost all the patients admitted for COVID-19 were unvaccinated, it said.
That echoes what Idaho hospital leaders, public health officials and data have said.
Younger people are getting sicker
The age of people hospitalized with COVID-19 has shifted.
Back in the late 2020 surge, more than half of Idahoans hospitalized with COVID-19 were 70 and older. But that age group turned out in droves at clinics and pharmacies and hospitals, looking to get a COVID-19 vaccine. Almost 80% of Idahoans 65 and older have gotten at least one dose of the vaccine, according to state vaccination data.
Since vaccines became widely available, a growing share of hospitalizations for COVID-19 in Idaho are in people under 60.

Hospitalizations among children for COVID-19 remain rare in Idaho.
Some physicians in other states have been outspoken in their belief that the virus poses a greater risk to children than it did before. That’s unproven, the Washington Post reported.
“What is indisputable is that in a swath of low-vaccination states stretching from Florida, South Carolina and Texas, up to Indiana and Missouri, the first large wave of pediatric cases is hitting hard — overwhelming hospitals, dominating political debates over mask and vaccine mandates and throwing school reopening plans into disarray,” the Post reported Friday.
The pediatric COVID-19 hospitalization rate in the U.S. is now higher than at any previous point in the pandemic, it noted.
Souza noted that the Treasure Valley has only one pediatric ICU, with just 12 beds.
And younger adults are getting sick, too.
A medical director who oversees ICU care at Saint Alphonsus Regional Medical Center told the Sun recently that she had patients in their 30s.
“Yesterday, I had a 37-year-old patient die of COVID,” she told the Sun in a late July interview.
Another patient in his 30s, sick enough to need intensive care, insisted from his hospital bed that the vaccine wasn’t safe and effective, she said.

